When Scientists Become Allergic to Their Research
This story was originally published in Undark and appears here as part of the Climate Desk collaboration.
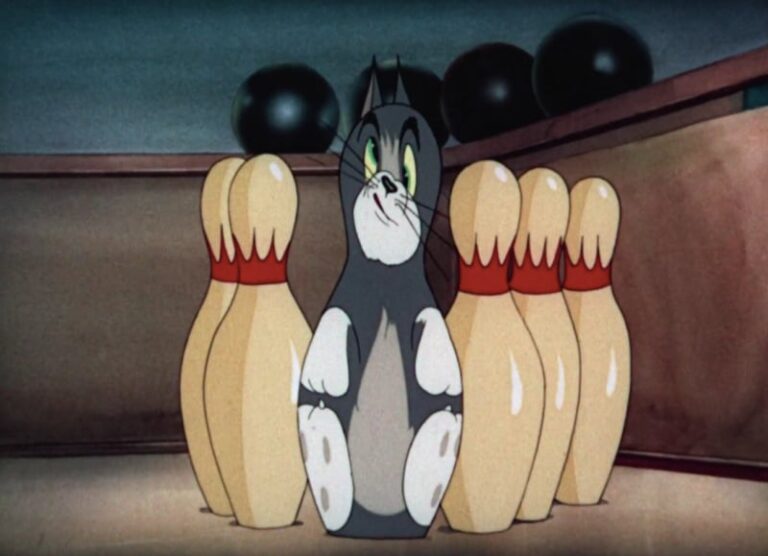
Bryan Fry’s heart was pounding as he stepped back from the snake enclosure and examined the bite marks on his hand. He had just been bitten by a death adder, one of Australia’s most venomous snakes. Its neurotoxin-laced bite could cause vomiting, paralysis and—as the name suggests—death.
Fry, at the time a graduate student, had kept snakes for years. Oddly, the neurotoxins weren’t his biggest worry; the nearby hospital would have the antivenom he needed, and, although data is limited, people who receive treatment generally survive. Anaphylactic shock, on the other hand, might kill him within minutes.
“Anaphylactic shock is the single worst feeling you can possibly imagine,” recalls Fry, now a biologist at the University of Queensland in Australia. “It is just insane. Every cell in your body is screaming out in mortal terror.”
Fry, who had spent his life admiring and eventually studying venomous snakes, had become deathly allergic to them.

While most cases are not so extreme, anecdotal reports and expert analysis suggest that it is far from rare for scientists, students, and laboratory technicians to develop allergies to the organisms they study. Perversely, some allergy researchers say, it is the researchers’ passion for their subjects—the close observation, the long hours of work each day, and the years of commitment to a research project—that puts them at such high risk.
“It is true that some things cause allergies more often than others, but the biggest factor is the frequency of the interaction with the study organism,” says John Carlson, a physician and researcher at Tulane University who specializes in insect and dust mite allergies. “You probably have about a 30 percent chance of developing an allergy to whatever it is that you study.” While data is limited, that estimate is in line with research on occupational allergies, which studies suggest occur in as many as 44 percent of people who work with laboratory rodents, around 40 percent of veterinarians, and 25 to 60 percent of people who work with insects.
Federal guidelines suggest that laboratories have “well-designed air-handling systems” and that workers don appropriate personal protective equipment, or PPE, in order to reduce the risk of developing an allergy. However, interviews with researchers and experts suggest that there may be little awareness of—or adherence to—guidelines like these. For scientists working with less-common species and those engaged in fieldwork, information on what exactly constitutes appropriate PPE may be very limited.
Many researchers, perhaps especially those who do fieldwork, are used to being uncomfortable in service of their work, Carlson points out. “I think that a lot of researchers are so interested in the process of the research,” he says, “that they aren’t really considering the long-term effects that it could have on them.”
In general, allergies develop when the immune system overreacts to a substance that is usually harmless, or relatively harmless. The immune system monitors the body for potentially dangerous invaders like bacteria, fungi, and viruses. Sometimes, for reasons that are not well understood, the immune system identifies something benign, like pollen or animal dander, as dangerous. To help mark the intruder, a person who has become sensitized in this way produces antibodies, or types of proteins, to identify it.
When that person comes into contact with the substance again, the antibodies flag it as an invader. As part of the response, immune cells release compounds like histamine, which irritate and inflame the surrounding tissues, resulting in allergy symptoms.
Although some risk factors have been identified, researchers who study allergies are often unable to determine exactly why this overreaction occurs in some people but not others. But it’s clear that, for some substances, repeated exposures can increase the likelihood of an allergic response.

After about a year and a half of this, she started to notice symptoms. At first, the bites became itchy, but the more she was exposed, the worse it got. “The last time I fed a leech—which I try not to do anymore—my entire hand swelled up so much that I could hardly make a fist,” she says. “It itched like crazy.” De Carle says that, when she’s out hunting leeches now, she can avoid an allergic reaction if she removes the leech after it attaches itself to her, but before it starts to feed. For the leeches she keeps in the lab, she’s switched to feeding them pig’s blood from a butcher shop instead of letting them feed on her.
Nia Walker, a Ph.D. student in biology at Stanford University, has also begun reacting to her research organism. Walker studies how genetics influence coral bleaching resistance and recovery. She began to notice rashes on her hands during her third trip to conduct fieldwork on corals in Palau, an island nation in the South Pacific. “And then each subsequent trip after that, it got more and more extreme,” she says. “It got to the point where my face would bloat and I’d get welts on my hands from touching them.”
While her symptoms are especially intense, Walker says she’s not the only member of her lab who has developed a sensitivity. By now, she says, everyone in the lab has “developed a slight irritation to corals.” Walker has been able to manage her allergy by using protective equipment and over-the-counter antihistamines. “It’s sad,” she says, “but it’s also pretty funny.”

In many cases, scientists report that their allergies are annoying but manageable. But sometimes, the allergies force researchers to make major changes.
Entomologist Chip Taylor began his career studying sulphur butterflies as a Ph.D. student at the University of Connecticut. When he started his own lab at the University of Kansas in 1969, he had every intention of continuing to work with the species. But, he says, “by the time it rolled around to 1973, I realized I was so allergic to these butterflies.” Taylor began to experience asthma-like symptoms whenever he worked with them.
In the summer of that year, during a research trip to central Arizona, Taylor and a colleague rented a trailer to use as a workstation to process butterfly wing samples. “I could not go in the trailer,” he recalls. “I slept outside with my back up against a tree so my sinuses and my throat could drain.” To manage his symptoms, he was regularly taking prednisone, a powerful anti-inflammatory drug that can have serious side effects. “I decided that I had to get out of working with those butterflies,” Taylor says. “I had to readjust my career to work on something else.”
Taylor spent the next few decades studying killer bees. He returned to butterfly research in 1992, when he started the monarch butterfly conservation program Monarch Watch. Taylor says he’s never experienced any symptoms while working with monarchs—maybe, he guesses, because the two species produce different types of pigments.

Fry, the biologist who became allergic to snake venom, also says his allergy has shaped his career. The venoms of different snake species share similar components, Fry says, so someone who is allergic to one type of snake is likely allergic to many types. Because of this allergy, Fry also has to be extremely careful even around venomous snakes that are usually not dangerous to humans.
“Whenever I work with these animals now, I look like I’m going into the Hurt Locker,” he says, referencing the Oscar-winning movie about U.S. Army specialists who defused bombs in Iraq. “So, of course, in the tropical sun I’m absolutely melting.” Those limitations, he says, have made working with snakes less enjoyable. “I can’t just blithely interact with these animals that I find so absolutely fascinating, knowing that death is just around the corner at any given moment, even from a snake that normally wouldn’t be a medical problem.”
Fry survived his encounter with the death adder thanks to a snakebite kit containing injectable adrenaline and antihistamines, as well as a quick-thinking friend who raced him to the hospital. The allergy, he said, has caused him to redirect much of his research to studying venoms in other animals, including Komodo dragons, slow lorises (the world’s only venomous primates), funnel-web spiders, and box jellyfish. “I’ve managed to turn it into a good thing,” he said, “but it’s been nevertheless very frustrating.”
Allergy experts say that reducing exposure is the key to preventing allergy development. Exactly how much the exposure needs to be reduced is less clear, and increasing protection may be costly for institutions and inconvenient for researchers.
Some laboratories that use mice and rats have equipment and policies designed to reduce exposure to allergens. These labs install ventilation systems for the cages, use a robotic system to clean them out, house fewer animals per room, and provide an area for workers to change out of allergen-contaminated clothing. PPE such as masks, gloves, and gowns can also help researchers reduce their exposure.
But actually applying those preventative measures can be challenging, says Johanna Feary, who studies occupational lung disease as a senior clinical research fellow at Imperial College London.
In 2019, Feary and several colleagues published a study of seven research institutions in the United Kingdom that performed research on mice. They found that facilities that used individually ventilated cages, instead of open cages, had dramatically lower airborne allergen levels. But even that was not sufficient to prevent technicians from becoming sensitized to mouse allergens. The facilities with the lowest levels of sensitization were those where workers also wore properly fitted masks. The research, she said, demonstrated that, at least in the U.K., the development of allergies to lab animals “is probably preventable in almost all cases.”
And with less well-studied allergies, there’s simply little information available regarding prevalence and what sorts of protections are sufficient to prevent their development. Several scientists living with allergies, though, say they think that more information and awareness could help increase the number of scientists taking precautions in their research.
Fry says there is more awareness of snake venom allergy than there was when he started formally studying snakes in the late 1990s. But, he added, “it’s still not as well-known as it should be.” Researchers in the field, he writes in a follow-up email, can be reticent to talk about venom allergies. But, he says, “I’m quite candid about it because, you know, this is life-saving information.”

Walker, the coral biologist, says more research on allergies among researchers would be helpful. “A lot of these things can be addressed if you knew to look out for it,” she says.
Early-career scientists generally receive thorough training on proper handling of biohazards and harmful chemicals. Institutions often provide extensive safety plans for fieldwork to help researchers prepare for the various risks involved, from dehydration to hypothermia to bear attacks. But scientists may learn little about the potential for developing allergies to seemingly harmless organisms.
“I feel like maybe there’s a bit too much of a casual attitude about protective gear,” says McGoey, who developed an allergy after doing research on ragweed. “Maybe especially if you’re working with a plant or animal, where it’s like a natural thing, and you’re not in the lab with a chemical, maybe people are just not careful enough.”
“As silly as it sounds, just maybe having more emphasis on using PPE and the consequences of not doing it would be kind of nice,” says de Carle, the leech researcher. “It can be really easy to just think, like, ‘Oh, I don’t really need to wear gloves; I’m just touching flowers or whatever.’”
Carlson, the allergist, says that even well-informed researchers can get caught up in their enthusiasm for the work and rationalize not taking the proper precautions.
In 2009, Carlson worked on a project that involved collecting data on house dust mites, microscopic arthropods which cause nasal and respiratory issues in millions of people worldwide. Despite his expertise, he neglected PPE. “I know all this,” he says. “I know I should be wearing a mask, but it’s hot, and it’s sweaty, and I don’t have a boss telling me what to do.” As he worked, he developed a runny nose and itchy eyes—the first steps toward a full-fledged allergy. “I pushed through and I ended up hyper-sensitizing myself,” Carlson says, to the point that even getting down on the ground to play with his then-young children made him “absolutely miserable.”
Carlson is saddened thinking about those scientists who have to give up the work they love due to allergies. “I really do feel for these folks doing their work and developing an allergy,” he says. “The more we get the word out there, the better.”